IBS vs. Colon Cancer: How to Tell the Difference
As with IBS, your doctor will want your complete personal and family medical history.
Risk factors may include:
- colorectal polyps
- Crohn’s disease
- familial adenomatous polyposis (FAP)
- family history of colorectal cancer
- hereditary non-polyposis colon cancer (HNPCC), also known as Lynch syndrome
- lack of physical activity
- poor diet
- type 2 diabetes
- ulcerative colitis
In addition to a physical exam, your doctor may order blood and stool tests. If cancer is suspected, other tests may include:
- colonoscopy, along with tissue biopsy
- imaging tests, such as X-ray or CT scan of the colon and rectum
The biopsy can confirm the presence of colon cancer and imaging tests can help assess whether the cancer has spread.
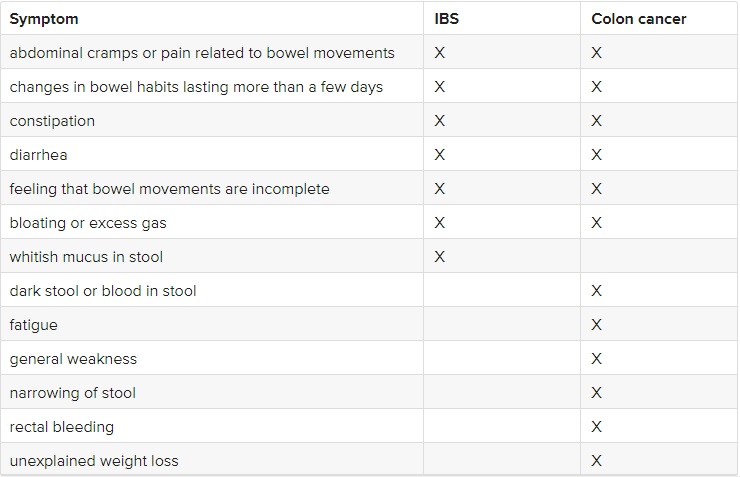
IBS vs. colon cancer symptoms
Although some symptoms of IBS and colon cancer are the same, there are some distinct differences to keep in mind. This chart shows how IBS and colon cancer are similar and how they differ.
Can IBS lead to colon cancer?
IBS, with all its discomforts and inconveniences, doesn’t cause damage to your digestive tract or lead to other health problems.
A 2010 trial found that when undergoing colonoscopy, people with IBS were no more likely to have structural abnormalities of the colon than healthy people.
They also found that people with IBS are at no greater risk of precancerous polyps or colon cancer.
When to see a doctor
Seek the advice of a doctor if you have any concerns about abdominal discomfort or changes in bowel habits. Symptoms of IBS can also indicate a variety of other conditions, including colon cancer.
Other signs that you should see a doctor right away include:
- persistent abdominal pain
- rectal bleeding
- vomiting
- weight loss
Having IBS doesn’t increase your risk of colon cancer, but that doesn’t mean you should ignore symptoms. To be on the safe side, tell your doctor about new symptoms such as rectal bleeding, narrowed stool, or weight loss.
Talk to your doctor about colon cancer screening. For most people, colonoscopy screening should begin at age 50.
If you have a family history of colon cancer or other risk factors, your doctor may recommend earlier or more frequent screening.
IBS can generally be managed by making certain dietary and other lifestyle changes. More severe cases can be treated with medications.
Having IBS doesn’t increase your risk of developing colon cancer.
Symptoms of colon cancer tend to appear only after the disease has spread. Screening for colon cancer can detect and remove precancerous polyps before they have the chance to develop into cancer.
Because the symptoms of IBS, colon cancer, and some other gastrointestinal disorders overlap, see a doctor to get the right diagnosis. They can help you manage or treat your condition so you can start feeling better.